Chemical injuries to the eye represent one of the true ophthalmic emergencies, wherein time is truly crucial. While almost any chemical can cause ocular irritation, serious damage generally results from either strongly basic (alkaline) compounds or strongly acidic compounds. Alkali injuries are more common and more clinically challenging as they damage deeper tissues with a significant potential for long term morbidity. Bilateral chemical exposure is especially devastating often resulting in complete visual disability [1].
Immediate prolonged irritation followed by aggressive early management and close long term monitoring is essential to promote ocular surface healing and to provide the best opportunity for visual rehabilitation.
Case Report
 A 19 year old female patient weighing 50 kgs presented to us with history of acid burns which was thrown on her face due to personal enmity. She had first aid elsewhere before she flew down to our institution.
A 19 year old female patient weighing 50 kgs presented to us with history of acid burns which was thrown on her face due to personal enmity. She had first aid elsewhere before she flew down to our institution.
On examination, she had completely disfigured face & chemical burns had affected neck, upper part of chest and both upper extremities upto elbow. The ventral aspect of upper extremities were injury free. The mouth opening was hardly one finger, so Mallanpatti score could not be assessed. She was a known asthmatic and was taking Budecort inhaler 2 puffs twice a day. Her vitals and hemogram were unremarkable. ECG and Echo were normal. Room air SpO2 was 96-97%. Systemic examination showed scattered rhonchi and crepitations bilaterally. With these findings, we proceeded with our plan to take her for surgery as even an ambulatory vision in these patients is a remarkable achievement.
Patient was asked to continue her bronchodilator inhaler preoperatively. She was already on Tablet Augmentin (Amoxycillin and Pot. Clavulunate ) 675mgs twice a day started 2 days preoperatively. The patient was premedicated with Injection Glycopyrolate intramuscularly one hour preoperatively. In the preoperative area a venous access was established with an 18 G cannula on the ventral aspect of left forearm. Patient was nebulized with Ketamine 5mgs in 5 ml distilled water and was wheeled inside OR. Monitoring included ECG, NIBP, ETCO2, SPO2 and temperature. Saturation has improved 98-99% with no rhonchi and very few crepitations on auscultation. As airway was difficult, an awake fibrio optic intubation was planned. The patient was explained the procedure clearly. She was given lignocaine lozenges half an hour before procedure to anaesthetize oral cavity and reduce gag reflex. Nasal cavity was packed with 2% lignocaine and adrenaline soaked ribbon gauze for 15 minutes. This was subsequently removed and nasal cavity and endoscope was well lubricated using 2% Xylocaine jelly. As nasal cavity also had the brunt of the burns, it could take only a 6 mm flexometallic endotracheal tube which was threaded to endoscope. Patient was given IV Midazolam 1 mg, IV ondansetron 8 mgs and IV Fentanyl 30mcgs. The scope was slowly introduced down the nasal cavity without trauma and all the structures were clearly visualized. The patient was very cooperative as there was no gagreflex. On visualization of vocal cords, 2% Xylocaine was sprayed on the cords and the endoscope was introduced upto carina and the flexometallic tube was threaded into trachea. The endoscope was slowly brought out and closed circuit was connected to the ET tube. The correct placement of the tube was checked by Auscultation and Capnograph.
Propofol 2mg/kg, Fentanyl 30mcgs and Vecuronium 1mg/kg were given intravenously and connected to ventilator.
The patient was maintained on 3% Desflurane for the duration of 4.5 hours. IV Hydrocortisone 100mgs was also given. An infusion of Dexmedetomidine ( 0.5mcg/kg/hr) was started using an infusion pump and continued till half an hour before the end of the procedure. Her vitals were unremarkable. At the end of the surgery the residual paralysis was reversed with Neostigmine and Glycopyrolate. Patient was extubated when she was completely awake and obeying the commands.
DISCUSSION
OOKP is a complex 2 stage operation which aims to restore vision to the most severe cases of corneal and ocular surface patients for whom all previous attempts to restore vision has failed. The procedure involves removing a canine tooth from patient, shaping and drilling it to allow implantation of an artificial plastic corneal device (Optical Cylinder) and ultimately implanting it back into the eye a few months later.
Summary of OOKP Surgical Procedure
 Stage I involves 5 separate procedures
Stage I involves 5 separate procedures
- Opening up one eye and removing the entire inner surface of the eyelids, corneal surface and all scar tissue from previous eye injury.
- Removing inner mucosal lining of the cheek and transplanting it on the new surface of the eye.
- Removing the canine tooth and part of the adjacent bone and attached ligament from the jaw.
- Fashioning a bolt shaped structure from the tooth bone complex to receive the plastic optical cylinder which is cemented into place.
- Implanting the tooth-bone-cylinder complex into a submusculer cheek pouch to grow a new blood supply.
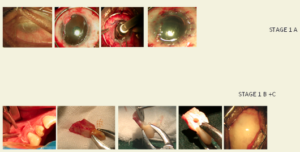
Stage IA – Preparation of Mucous Membrane covering
Stage IB – Preparation of Globe
Stage IC – Preparation of Lamina
Stage II is undertaken about 3-4 months later. It has two separate procedures.
First the cheek mucosal lining over the eye will be opened, a circular opening made in the cornea to receive the implant. The inner contents of the eye will also be removed at the same time.
Secondly, the living tooth bone cylinder complex will be removed from the cheek and placed within the eye. The mucosal cheek lining is replaced over the implant. At the end of the procedure, light can enter through plastic cylinder and patient gets a good vision if retina is healthy.
Indications for OOKP
SJS [2,3], Ocular cicatrial graft failure, bilateral corneal blindness (LYELL Syndrome) [4,5] Ocular cicatrial pemphigoid, chemical burns, end stage trachoma, dry eyes.
Post Operative complications – To enumerate a few
Endophathalmitis [6], loss of cylinder / lamina, Glaucoma [7], choroidal / retinal detachment [8], infection of lamina in pocket, absorption of lamina, expulsive haemorrhage, vitreous haemorrhage, expulsion of cylinder / prosthesis
Conclusion

 Thus OOKP is a multi disciplinary team effort, needs a good counselling of patient, proper understanding of patients systemic condition and comorbidities and a well drafted anaesthetic plan to enable the patient to get a decent vision.
Thus OOKP is a multi disciplinary team effort, needs a good counselling of patient, proper understanding of patients systemic condition and comorbidities and a well drafted anaesthetic plan to enable the patient to get a decent vision.
REFERENCES
-
Falcinelli G, Falsini B, Taloni M, Colliardo P. Modified osteo-odonto-keratoprosthesis for treatment of corneal blindness: Long term anatomical and functional outcomes in 181 cases. Arch Ophthalmol 2005; 123: 1319-29.
-
Liu C, Paul B, Tandon R, Lee E, Fong K, Mavrikakis I, et al. The osteo-odonto-keratoprosthesis(OOKP). Semin Ophthal 2005; 20:113-28.
-
Reddy SC, Tajunisah I, Tan DT. Osteo-odonto-keratoprosthesis in Stevens-Johnson syndrome. A case report. Int J Ophthalmol 2011; 4: 212-5.
-
Falcinelli G, Missiroli A, Pettiti V, Pinna C. Osteo-odonto-keratoprosthesis uptodate. Acta Concil Ophthalmol 1987; 25:2772-6.
-
Viitala R, Franklin V, Green D, Liu C, Lloyd A, Tighe B. Towards a synthetic Osteo-odonto-keratoprosthesis. Acta Biomater 2009; 5: 438-52.
-
Pintucci S, Pintucci F, Sarra A. PMMA/Dacron biointegrated keratoprosthesis 19 years experience. An Inst Barraquer(Barc).2001;30:97-99.
-
Netland PA, Terada H, Dohlman CH. Glaucoma associated with keratoprosthesis. Ophthalmology 1998; 105:751-757.
-
Nadal J, Barraquer J. A new lens for vitreous and retinal surgery in osteo-odonto-keratoprostheses patients. An Inst Barraquer(BARC) 2001; 30: 71-74.